Do I Have Binge Eating Disorder? Signs, Symptoms & Treatment

There is a feeling of guilt and shame around the binge-eating episodes.
Binge eating disorder (BED) is the most common eating disorder in the U.S., affecting about 3% of the population at some time in their lives. Of people with eating disorders, 47% have binge eating disorder. BED is characterized by recurrent binge eating without compensatory measures to counteract the binge, such as purging, laxative overuse, and exercise found in binge-purge disorder. Binge eating disorder often goes untreated due to a lack of understanding and the secrecy associated with the condition. Significantly, binge eating impacts day-to-day life and health with the increased potential for cardiovascular disease, diabetes, chronic pain, and more.
We sat down with Sanford Comprehensive Treatment for Eating Disorders (SCTED) Director Lori Kehoe, MA, to discuss binge eating disorder and its connection to substance use and other mental health conditions.
Binge Eating Disorder with Lori Kehoe, Director Sanford Comprehensive Treatment for Eating Disorders

Director Eating Disorder Services, Lori Kehoe, MA
SBH – What are the signs and symptoms of a binge eating disorder?
LK – With BED, we have symptoms that indicate binge eating is out of control. The person is unable to control the amount of intake. They eat when they are not hungry and to the point of discomfort. One of the indications will most often be that they are eating alone. They are in seclusion. That is their ritual, and there is a feeling of guilt and shame around the binge-eating episodes.
When determining signs and symptoms, first look at behaviors. You might notice fluctuations in weight if you are close to the person. As a family member, support person, or roommate, you will begin to find wrappers hidden in couches. You will find multiple containers hidden in their room, and there are often rituals around purchasing in bulk and hiding those items. Large amounts of food may be missing from the pantry. You may even notice money missing from your wallet or bank account.
The behavior is both impulsive and calculated. The patterns are similar to drug or alcohol addiction. The person will pull away from dining together and most social situations. Eventually, they become so ashamed and consumed that BED leads to missing school, work, or important milestones.
SBH – What causes binge eating disorder?
LK – The biological, psychological, and social influencing factors are the first things we want to look at when assessing a person for the best treatment plan at SCTED. How did this person grow up? Were they raised in a home that lacked food? Did they grow up with basic needs met: nutrition? Was this person restricted from certain foods? In some households, there are “good” and “bad” foods; children are never allowed candy or special foods like cake on a birthday. Conversely, did they grow up in a home where there was an issue of gluttony?
We have to look at lifelong patterns that began in childhood. Were they overfed or underfed as children? And then, we start to look at their values regarding physical appearance and what matters to them. We look at their relationship with themselves and others, their feelings of adequacy or inadequacy, Do they suffer from depression? Have they had traumatic events in their lives?
SBH – It sounds like adverse childhood experience is a significant factor.
LK – Absolutely. 60% of people who take the adverse childhood experience questionnaire (ACEs) will have at least one negative childhood experience, and 16% have at least four. ACEs are linked to a higher likelihood of health challenges later in life. Consequently, food can become a drug used as medication. It can numb your body and brain. So we must find out what bingeing is doing to meet the person’s psychological needs. There are many reasons why a person with a binge eating disorder uses food to fill the need.

Building a healthy relationship with food at Sanford Comprehensive Treatment for Eating Disorders
SBH – Can a restrictive diet trigger a binge eating disorder?
LK – Restrictive dieting or restriction most often leads to eating disorders in general. One might routinely restrict food and, after a period of time, engage in a binge episode. That may lead to a variety of eating disorder diagnoses. Often we see restriction leads to compensatory behaviors such as laxative abuse, purging and over exercise, which is bulimia nervosa. Recurring binge episodes without compensatory behaviors is characterized as binge eating disorder.
SBH – Do you have a case study you could share?
LK – We have a case of a person with a previous substance use disorder diagnosis. This person was out of control with their substance of use for years but went into addiction treatment (not at Sanford) and was abstinent in recovery. They had experienced trauma and used drugs and alcohol to numb the pain. However, after treatment, they found themselves using food for comfort, and some of the same hiding and secretiveness patterns emerged. They had not gotten to the root cause of their addiction, and their need to “fill that hole” persisted. Our clients may go through a grief process in treatment because food has become a best friend and fills a need.
SBH – How do we educate the public about the severity of BED?
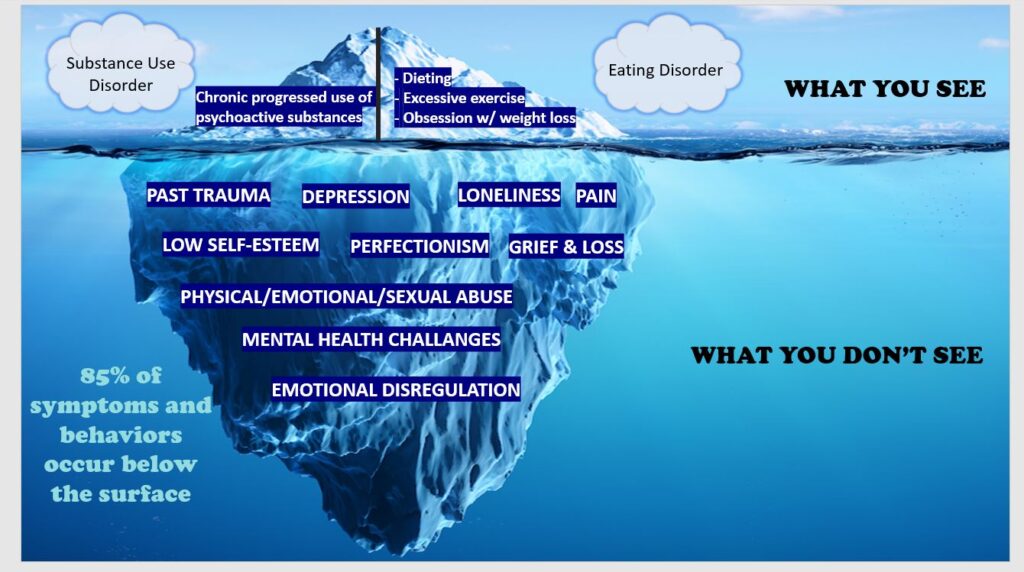
LK – I am so glad you asked that question. We must help our community understand that treatment is necessary for a binge eating disorder. It is an addiction as severe and life-threatening as other eating disorders. Sanford Founder Rae Green and I go on the road, giving a presentation on the connection between substance use disorders and eating disorders. We are trying to build awareness, reduce stigma, and help people identify the signs. I use an iceberg diagram as an example of what you see and what lies below the surface.
SBH – What treatment is used at SCTED to treat BED?
LK – There are many approaches we can take because we have many specialists here. We start with a medical and psychiatric assessment from our psychiatrist-led medical team. Nutritionists monitor supplements and vitamins, hunger and fullness cues, provide meal support and build a healthy relationship with food. And, of course, clinical getting to the root cause, teaching our BED clients to enrich themselves rather than fill themselves with food. Recreational therapists provide real-life experiences in the safety of treatment.
,
At Sanford, we use an integrated treatment approach. We treat the whole person with a psychiatrist-led interdisciplinary team. There should not be surprises like the case study I mentioned because we expect mental health crossovers. We also can diagnose and treat co-occurring disorders under one roof.
SBH – Anything else you would like to tell us about eating disorders?
LK – Yes. We all have different bodies, and valuing and respecting that is vital. Similarly, there is more to value than our appearance! We have a social media group and a body diversity group at SCTED to focus on those points. We offer individual and family therapy, but group therapy works well for several reasons.
First, people need education and awareness. They need to come to treatment and leave with tools – group therapy helps develop the toolkit. Next, our clients are with their peers and realize they are not alone. Lastly, the power of the group comes from support and connection. The connection in the group catapults the effectiveness of treatment and its microcosm of the world outside in recovery. Treatment is the place to practice what you can do in your world when you go home.




