The Parallels Between OCD and Eating Disorders
Researchers have speculated on the parallels between OCD and eating disorders since the 1930s.
Last week was OCD Awareness Week, and we sat down with Sanford Comprehensive Treatment for Eating Disorders (Sanford CTED) Lori Kehoe, MA, to discuss the parallels between OCD and eating disorders. Studies show that individuals with eating disorders have 11 – 69% higher rates of OCD, and those with OCD have a 10 – 17% higher rate of eating disorders. 64% of those with eating disorders and 41% with OCD also have at least one anxiety disorder (International OCD Foundation).
“We are fortunate at Sanford CTED to utilize all our resources under one roof at Sanford West Behavioral Health Campus. We treat co-occurring diagnoses with an integrative treatment approach. To experience full recovery, you can’t just whack a mole. Looking at the whole person, their entire history, and including their loved ones garners the best outcomes in mental health recovery.” Lori Kehoe, MA, Sanford CTED

Lori Kehoe, MA
OCD and Eating Disorders
SBH – How important is individualized treatment for co-occurring disorders like OCD and eating disorders?
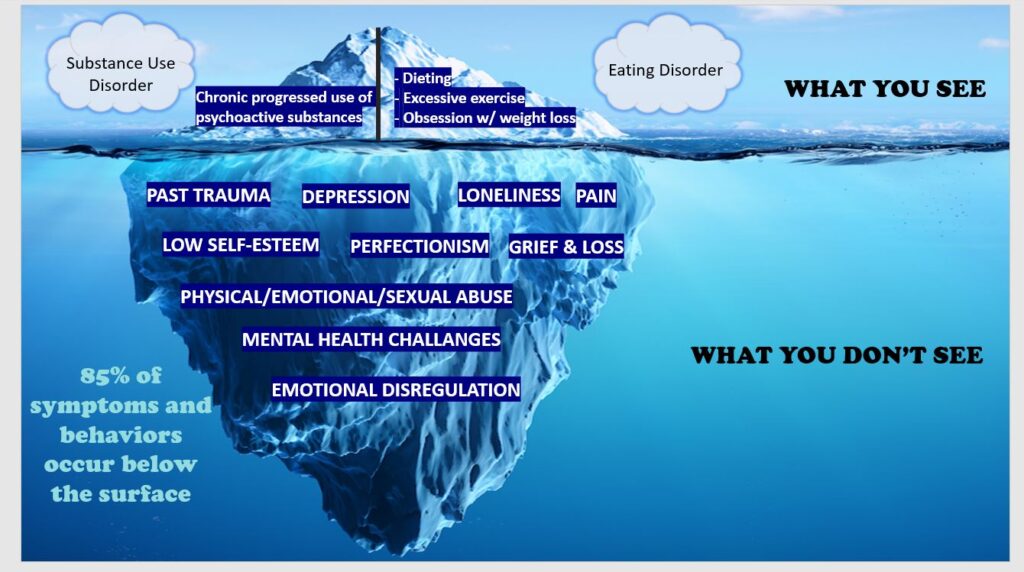
LK – Very – one of the things that allows us to interrupt the predictability of these diseases becoming fatal is getting to the underlying causes. At Sanford CTED, we look at the comorbidity of obsessive-compulsive disorder (OCD), eating disorder, and substance use disorder. We go to the iceberg graphic with a combination of all three because we have to get to the underlying root cause.
Genetics, environment, and brain chemistry are factors.
Genetics, environment, and brain chemistry are factors in all three disorders. With OCD, there is a pattern of unwanted thoughts and fears. Those are the obsessions that lead one to repetitive behaviors or compulsions. So when you think about OCD as an obsession with symmetry, the obsession that it has to be a certain way, you see how that leads to the compulsion to correct.
SBH – How are OCD and eating disorders connected?
LK – OCD and eating disorders are often accompanied by anxiety and depression. The connection between OCD and eating disorders is in avoidance of discomfort and avoidance of anxiety. When a person comes into Sanford CTED with OCD and an eating disorder, we’ve got to look at how the OCD began alongside finding out how the eating disorder began. Many obsessive thoughts and compulsive behaviors begin when an individual is young as a reaction to an adverse childhood experience and the resulting PTSD and trauma they experienced.
So, if we’re looking at the person’s story, we will go back to before the onset of the eating disorder. We will likely see a combination of rumination of thoughts, fears and feelings and some type of compulsive behavior. And we can talk to families to find out the patterns.
SBH – How do OCD and eating disorders manifest?
LK – Research has examined similar cognitive, behavioral, and personality characteristics in people with OCD, eating disorders, and SUD. Again, they offer this feature of repetitive thoughts and preoccupations. With an eating disorder, it will be a preoccupation and hyper-focus on food, body, image, and weight. With OCD, you’ll see obsessive preoccupation with symmetry, contamination, etc. The preoccupation will always be followed by a negative thought or effect – anxiety, fear, shame, and guilt. The behavior is intended to soothe these effects.
One of the things that differentiates eating disorders from OCD is that the person with an eating disorder often continues the repetitive thoughts, feelings, and behaviors with a denial of the devastating consequences. They don’t always see that it is something negative. But with OCD, their repetitive thoughts, obsessions, and compulsions are more obviously negatively impacting their daily life. When people accept that their life is unraveling and enter treatment, they begin to see that these obsessions, compulsive thoughts, and behaviors are interfering with real life.
To put it into perspective, we do see patients who have been washing their hands till they bleed or tapping or praying before they walk through a door, or restricting food or purging, and drinking till they blackout. They may also have panic attacks or high anxiety. At Sanford CTED, we understand that we must look at all the co-occurring issues. This means the primary, secondary, and tertiary disorders.
SBH – How do we get the word out about co-occurring OCD and eating disorders?
LK – I think it’s vital for us to get out in the community and talk about comorbidity and the influencing factors of OCD, eating disorders, and substance use disorders. Sanford founder Rae Green, Dr. Anna Flores, and I have a presentation we give to mental health professionals called Insatiable Hunger – The Shared Risk Factors of SUD and Eating Disorders. We include OCD as a prevalent co-occurring disorder to these conditions.
SBH – How are OCD and eating disorders treated?
LK – We can successfully treat OCD with evidence-based therapeutic modalities, medication, and alternative therapies offered at Sanford Behavioral Health. Some very effective therapies include comprehensive cognitive behavioral therapy, EMDR, somatic neuropsychotherapy, exposure-response therapy (ERP), and experiential therapy. Indeed, we have three eating disorder therapists in ERP training now. With somatic neuropsychotherapy, we go from the body to the brain instead of the reverse. This serves to release anxiety and trauma from the body systems stored over time.
The Sanford CTED team will look at all the harmful behaviors interfering with daily life. We have to begin to work on what thoughts and feelings are coming up right before I “have to” wash my hands, for example. We could use a diary card to write down the feelings and thoughts that occur before the obsessive, compulsive behavior is triggered. This is what I was thinking before I wanted to go to the bathroom and purge.
It begins with awareness. We talk about awareness all day and how we can change the behavior. It is a step-by-step process. There is constant supervision, support, and encouragement. It is also individualized treatment. We are helping them let go of repetitive patterns and develop healthy habits. If we can get to the root cause of why these thoughts and feelings are happening, we can release them before the compulsive behavior happens. We take it day by day.
Sanford CTED recreational therapists are prepping for “Spooky Week” and experiential excursions.
SBH – What does recovery look like for someone with OCD and an eating disorder?
LK – Recovery is a process. That is why the continuum of care is very important. When we think about recovery from eating disorders and OCD or other comorbid diagnoses, we must take our time because there’s a lot to unpack. When you have integrative treatment, you are going down the continuum of care. You’re not rushing from a 30-day stay in residential to outpatient providers.
It’s so important at the residential level to complete that level of care and to step down gradually. Sanford CTED has day programs (PHP), half-day programs (IOP), and telehealth for family and alumni programs. This provides continuity and a solid group that includes a primary care provider, psychiatrist, physician, dietitian, and therapist specializing in eating disorders and co-occurring diagnoses.
SBH – Anything else?
LK – If we can, as humanity, we should look at our lifetime as a classroom. Recovery is a practice. We are not alone; we have a community. It is good to take advantage of the resources in our community of like-minded people. Being part of organizations that help support you being connected is vital to recovery. We are fortunate at Sanford CTED to utilize all our resources under one roof. We can treat everything at the same time. To enjoy full recovery, you can’t just whack a mole. Looking at the whole person, their entire history, and including their loved ones garners the best outcomes in mental health recovery. I am proud to work for an organization that understands that maxim.